There are a few different terms people use to describe experiences that feel removed from usual life: dissociation, depersonalization, and derealization are three of the most common.
Simply put, dissociation is a general term describing a disconnection from one’s environment or thoughts, and depersonalization is the specific feeling of experiencing one’s thoughts and feelings as if from a distance. When we talk about derealization, on the other hand, we’re talking about the experience of becoming detached from one’s surroundings—a feeling of disconnection from reality itself. This could manifest as a distorted perception of time, space, and people, as well as a feeling of being in a dream or fog.
While it’s not entirely understood, derealization is believed to be a defense mechanism the brain uses to protect itself from overwhelming emotions or experiences. Several things can activate this defense mechanism, causing us to feel that we’ve suddenly stepped outside of the reality we know, including stress, trauma, depression, and drug use.
In this article, we’ll look at how a misunderstood mental disorder called Obsessive-Compulsive Disorder (OCD) may also result in this destabilizing symptom. We’ll discuss the types of OCD most closely associated with the phenomenon and explain how the gold standard treatment for OCD—exposure and response prevention therapy (ERP)—can help reduce derealization and all other OCD symptoms.
OCD explained
Before we get into how OCD can cause derealization, let’s first get a handle on what OCD is and how it can impact the lives of people living with it.
Though often mischaracterized as an unreasonable desire for order or cleanliness, OCD is a serious mental health condition characterized by obsessions and compulsions.
Obsessions are persistent and intrusive thoughts, images, or impulses that cause distress or anxiety, while compulsions are repetitive behaviors or mental acts that are performed in response to the obsessions, in order to reduce distress or prevent something bad from happening. Obsessions and compulsions combine to make symptoms worse over time through something called the OCD cycle.
The OCD cycle
Everyone experiences random thoughts from time to time that leave them wondering: “Where did that come from?” But regardless of how bizarre or depraved these intrusive thoughts, urges, and images are, a person without OCD will likely dismiss them quickly without being too bothered.
People with OCD, however, tend to fixate on these random thoughts and seek meaning in them. They begin to obsess over what a fleeting intrusive thought about, say, stabbing their partner with a kitchen knife, says about the likelihood of carrying out such a heinous act.
Paradoxically, when you have OCD, having an intrusive thought or urge to do something awful means the likelihood of you acting upon it is exceedingly low. That’s because, cruelly, OCD latches on to what you care most about.
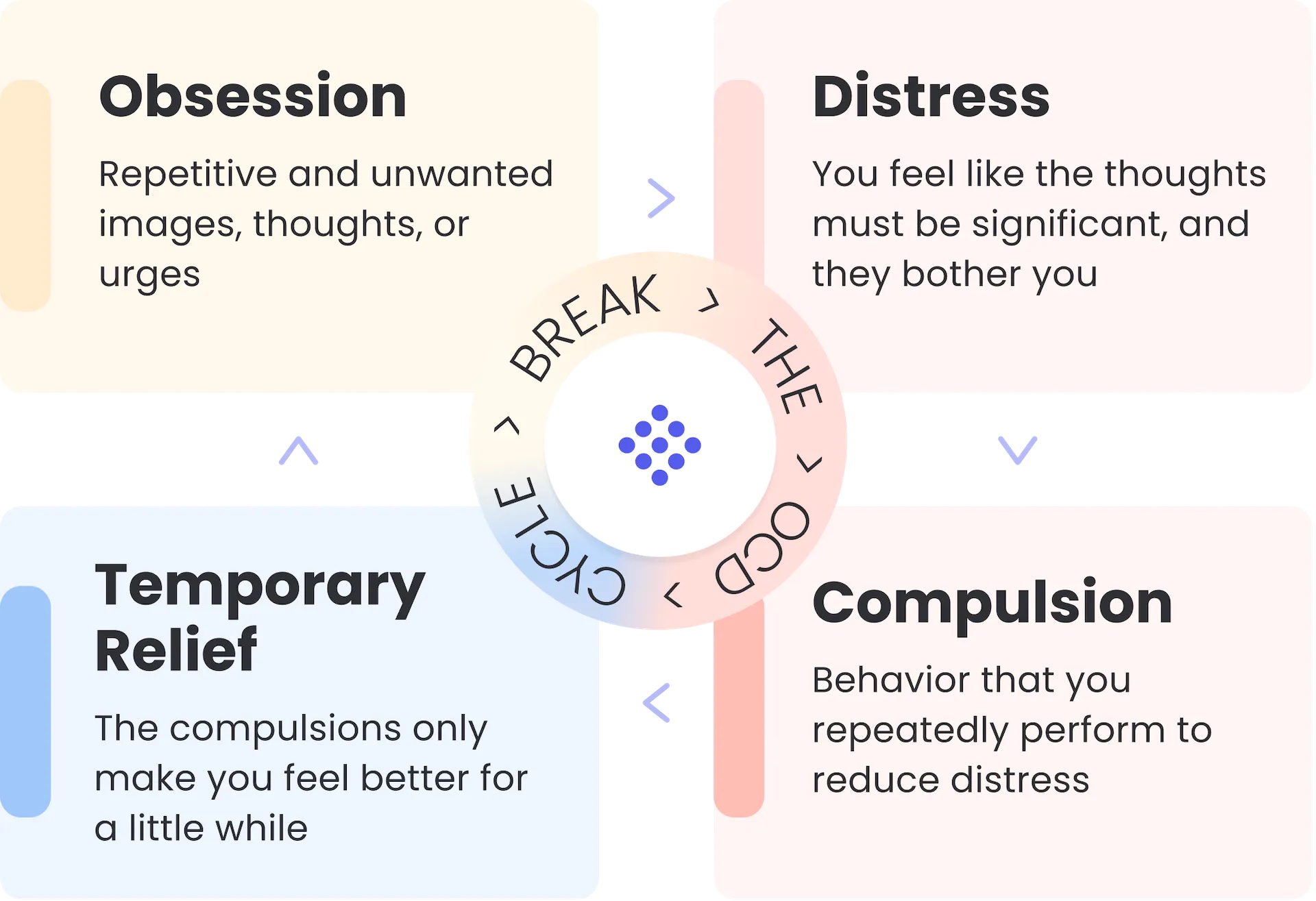
These obsessive thoughts are the first stage of the cycle. The second is the anxiety that they cause. To continue with our example, this person becomes anxious about the possibility of harming their partner. To quell this disturbing anxiety, they seek certainty that such a thing could never happen. And to find that assurance, the person arrives at the third stage of the cycle—compulsions.
Compulsions are simply behaviors intended to reduce the discomfort associated with obsessions. In our example, these compulsions could include removing every knife in the kitchen, researching the incidence of domestic stabbings on the internet, or avoiding being in the kitchen at the same time as their partner. There’s no end to the number and type of compulsions this person could engage in to resolve their doubts. Not for nothing, OCD is sometimes known as “the doubting disorder.”
These compulsions deliver relief from distress, but only for a short while. In fact, this fourth stage—relief—only perpetuates the cycle, as it reinforces the idea that something terrible will happen if compulsions aren’t done.
Because of this cycle, OCD tends to get worse and worse when left untreated, regardless of which form it takes. The example above would be categorized in the subtype of Harm OCD, as the sufferer’s fear is centered on the prospect of harming someone else. Here are just a few examples of other common OCD subtypes, though obsessions can involve any theme whatsoever:
- Contamination OCD: Excessive fear of contamination or germs, leading to compulsive cleaning, avoidance of certain objects or places, and heightened hygiene rituals.
- Order and Symmetry OCD: Obsession with symmetry, order, and exactness, resulting in compulsive behaviors like arranging objects in a particular way or repeating tasks until they feel perfect.
- Harm OCD: Persistent and intrusive thoughts or fears of harming oneself or others, accompanied by compulsive behaviors to prevent harm.
- Religious or Moral OCD (Scrupulosity): Obsessions related to religion, morality, or ethics, often involving excessive guilt, fear of sinning, or doubt about moral correctness, leading to rituals or excessive religious practices done out of fear.
- Relationship OCD: Obsessive doubts, fears, or uncertainties about romantic relationships, leading to repetitive reassurance-seeking, analyzing behaviors, and seeking proof of love or compatibility.
- Existential OCD: Intense fixation on existential questions and uncertainties, such as the purpose of life, the nature of existence, or one’s own mortality, resulting in persistent rumination, philosophical obsessions, and compulsive rituals aimed at finding answers or alleviating existential anxiety.
It’s estimated that OCD affects around 1-2% of the worldwide population, and it is equally prevalent in men and women. The exact cause of OCD is unknown, but it is believed to be a combination of genetic, environmental, and neurobiological factors.
So, now we have a general understanding of what OCD is and what it can look like, let’s dive into its connection to derealization.
Derealization and OCD
As we said at the beginning, derealization is believed to be a defense mechanism the brain uses to protect itself from overwhelming experiences and emotions.
“I’ve certainly seen my fair share of people who’ve experienced derealization as a symptom of their OCD,” says OCD therapist Jennifer Shafi. “Some people describe their experience as a feeling of non-reality like they’re in “the Matrix.” Others talk about being away from their body and not experiencing what is real and present.”
Shafi mentions two OCD subtypes most likely to cause derealization in people. The first of those is Existential OCD.
In Existential OCD, constant rumination and obsession with unanswerable questions and existential dilemmas can lead to an overwhelming sense of dread and a distorted perception of reality. The intrusive thoughts and doubts about the nature of existence can create a significant cognitive load and disrupt one’s ability to engage fully with their surroundings.
Furthermore, people with Existential OCD often experience heightened anxiety and constant unease related to existential concerns. This chronic state of anxiety can contribute to people experiencing derealization as an unintentional coping mechanism, where the mind attempts to distance itself from the distressing thoughts and emotions.
Shafi adds that Somatic OCD can cause derealization in some people due to the nature of the obsessive thoughts and the resulting anxiety.
“Somatic OCD involves obsessive concerns about bodily sensations, functions, or health,” she explains. “These obsessions can lead to excessive worry and fear regarding physical symptoms or the interpretation of bodily sensations.”
The intense preoccupation with bodily sensations and health-related concerns can create a heightened state of anxiety and distress. This chronic anxiety can trigger a dissociative response, such as derealization, as a way for the mind to cope with the overwhelming emotional and cognitive load.
It’s worth mentioning that derealization is far from a guaranteed experience for everyone with these types of OCD. Personal coping strategies, underlying psychological tendencies, and the severity of OCD symptoms can influence each person’s unique experiences and symptoms.
The impact of derealization and OCD
Derealization can significantly impact the quality of life of people with OCD. It can make it difficult for people to function normally in work, school, and family, and can interfere with their ability to form and maintain meaningful connections with others. It can also lead to feelings of hopelessness and despair as the person feels disconnected from the world around them.
People with OCD and derealization may feel trapped in a cycle of anxiety and disconnection, which can be difficult to break out of without proper treatment. The proven most effective therapy for derealization and all other OCD symptoms is exposure and response prevention therapy (ERP).
Reducing OCD-related derealization with exposure and response prevention therapy (ERP)
ERP focuses on gradually exposing people to situations or triggers that produce distressing obsessions or feelings of derealization. This exposure is done in a controlled and systematic manner, guided by a therapist. The goal is to help people learn to tolerate distressing sensations and thoughts associated with derealization without resorting to avoidance or safety-seeking behaviors, which only make their distress worse.
During ERP, a therapist will encourage you to intentionally and gradually expose yourself to situations or engage in activities that elicit feelings of distress or detachment. The therapist supports you in resisting the urge to escape or engage in compulsive behaviors to alleviate the discomfort. This process helps people with OCD learn that these distressing experiences are not dangerous or harmful, and that they can tolerate them without needing to engage in compulsions or avoidance.
Over time, with repeated exposure and the prevention of the usual compulsive responses, you’ll gradually habituate to the sensations of derealization, or the distress that leads to them. As a result, the intensity and frequency of derealization episodes can diminish, leading to a reduction in distress and greater freedom to live life on your terms.
Getting help
If you think you might have OCD and want to learn how it’s treated with ERP, I encourage you to read more about NOCD’s specialized, accessible approach to OCD treatment.
All of our therapists specialize in OCD and receive ERP-specific training. You can also get 24/7 access to personalized self-management tools built by people who have been through OCD and successfully recovered.
